Dr. Freeman: “Mr. Vargas, great news on the biopsy results: all negative. It means the workup we have done, including imaging, blood work, and endoscopies, is all normal. You’re all set.”
Mr. Vargas: “How can that be? I feel miserable!”
What are disorders of gut-brain interaction?
The clinical scenario above (names altered for privacy) is surprisingly common for gastroenterologists. These doctors of the esophagus, stomach, small intestines, colon, pancreas, and liver are well trained to identify and treat conditions of the gastrointestinal (GI) tract that occur from diseases caused by inflammation, infection, or cancer.
While some of these conditions can be devastating, they are usually easy to diagnose on standard testing. But there are other illnesses that can impact the GI tract that do not have a clear laboratory test or finding on endoscopy to identify them. One such class of these is called disorders of gut-brain interaction, or DGBIs. Some people (including doctors) may be familiar with the older term used to describe these conditions — functional GI diseases — but it is no longer used.
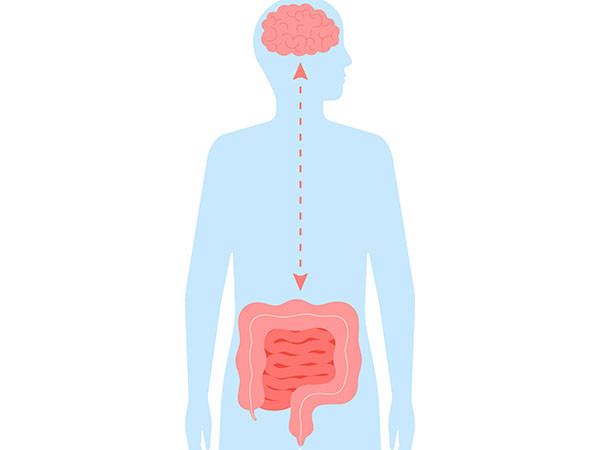
DGBIs can include irritable bowel syndrome, reflux hypersensitivity, or functional dyspepsia. They are called disorders of gut-brain interaction because it is believed the most critical abnormality is impaired communication between the gut and the brain via the nervous system in both directions (from gut to brain and brain to gut).
What can cause a DGBI?
Some things are associated with the development of DGBIs, including having suffered from prior infections, particularly those that have symptoms like nausea or diarrhea. DGBIs are more prevalent in certain populations, including women. Depression and anxiety are independent illnesses that can be associated with DGBIs as well. Unfortunately, the mechanisms of why DGBIs happen are still not well defined, which can be frustrating for patients and their providers.
From the perspective of specialists like me, DGBI management is not given a lot of attention in clinical training. This can lead to unnecessary testing that has risks, including perforation from endoscopy or radiation from imaging. Even more confusing is that DGBIs can overlap with other GI diseases. As an example, functional dyspepsia (a type of chronic indigestion) can overlap with gastroparesis (slow stomach emptying). Irritable bowel syndrome can overlap with inflammatory bowel diseases (like ulcerative colitis and Crohn’s disease).
What are the treatments for DGBIs?
DGBIs can be treated with multiple primary approaches, and these can also be combined: lifestyle, including dietary approaches; medications; complementary/alternative medicine approaches; and behavioral therapy. Lifestyle and complementary and alternative medicine approaches can be attractive options for some patients.
While eliminating very fatty and processed foods may improve GI symptoms when you have a DGBI, it is hard to sustain such severe changes in diet to control symptoms, and when done too strictly can lead to other conditions, such as feeding difficulties from avoidant restrictive food intake disorder.
Some people might try a low-FODMAP diet (this should be avoided if you’ve had an eating disorder). You can try to avoid FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols)-containing foods for one month (ideally guided by a doctor and/or a dietitian), and completely return to a normal diet if there is no improvement. If there is improvement, then add back foods systematically to make sure your diet is varied and provides all necessary nutrients.
Sometimes people consider acupuncture, ginger, turmeric, or herbal supplements, which you should always discuss with your doctor to prevent side effects or serious health issues, including liver problems.
Medication-based approaches typically use medications that have been used to treat conditions like depression, neuropathy, and fibromyalgia. Sometimes doctors do not clearly explain the rationale for using such medications; however, they are meant to improve the gut-brain interaction by improving pain sensation pathways in the brain, and perhaps even stimulating improved nerve function.
Finally, GI-directed behavioral therapies use cognitive behavioral approaches to improve GI symptom-specific anxiety with the help of a psychologist or therapist.
How can I talk about managing a DGBI with my doctor?
If your doctor has identified that you have a DGBI, make sure to emphasize how much it is negatively impacting your quality of life. For a condition like irritable bowel syndrome, the change in bowel movements and the associated pain can really cause daily distress. Many DGBIs can affect your ability to do certain types of work that may not allow you easy access to a bathroom. DGBIs also affect sexual health.
Make sure your provider understands that managing your DGBI is important, and you want to work together to find the right treatment approaches (or a combination of approaches), as discussed above.
Beyond this, it is important to recognize that DGBIs are established diagnoses, and are just as valid as any other gastrointestinal disease. When you have symptoms of a DGBI, it is not because of an issue of willpower or weakness, or ” just in your head.” These are disorders for which good treatments exist, and they can improve your symptoms and quality of life.